Epi Explained: What are Outbreak Investigations?
Outbreak investigations are systematic efforts undertaken by public health professionals to identify the source, cause, and control measures for disease outbreaks. These investigations aim to understand the who, what, where, when, and why behind a sudden increase in cases of a particular illness, enabling authorities to implement timely interventions to prevent further spread. Outbreak investigations are critical in managing infectious diseases, foodborne illnesses, and other public health threats, ensuring the safety of communities and minimizing the impact of disease outbreaks.
In this Epi Explained, we’ll explore the process, key steps, and importance of outbreak investigations (both in an ideal state and in more practical conditions), along with real-world examples.
Key Questions
What is an outbreak investigation?
An outbreak investigation is the process of identifying the source, cause, and spread of a disease outbreak. Public health officials use epidemiological tools to detect outbreaks, define cases, and implement control measures to prevent further transmission.
How do public health officials identify an outbreak?
Outbreaks are identified when the number of cases of a disease exceeds the expected baseline for a given population or time period. Public health authorities monitor disease reports and compare current trends to historical data to detect anomalies.
What are the key steps in an outbreak investigation?
The key steps in an outbreak investigation include verifying the outbreak, defining cases, conducting descriptive and analytical epidemiology, forming and testing hypotheses, implementing control measures, communicating findings, and monitoring ongoing cases.
What are some challenges in outbreak investigations?
Challenges in outbreak investigations include delayed reporting, incomplete data, multiple sources of exposure, and the need for international coordination during global outbreaks.
What are Outbreak Investigations?
An outbreak investigation is the structured process public health officials use to detect, investigate, and respond to an outbreak. An outbreak occurs when there is a higher-than-expected number of disease cases in a specific population, geographic area, or time period. Whether the disease is infectious (like the flu or COVID-19), foodborne (such as salmonella or E. coli), or even non-infectious (like chemical exposures), outbreak investigations help identify the source and prevent additional cases.
Outbreaks can occur in various settings, including hospitals, schools, workplaces, or the broader community. Rapid and accurate investigations are essential to controlling the spread of disease and protecting public health.
Key Steps in an Outbreak Investigation
Outbreak investigations typically follow a systematic approach to ensure that public health responses are evidence-based and effective. Here are the essential steps in the outbreak investigation process:
1. Verify the Outbreak
The first step is to confirm that an outbreak is occurring. This involves verifying that the reported number of cases is higher than the expected baseline for a particular population or region. Public health authorities compare current disease reports to historical data to determine whether the increase is statistically significant.
Example: During flu season, an uptick in flu cases may be expected. However, if a cluster of flu-like illnesses is detected outside the usual flu season or the number of cases is significantly higher than anticipated, this could signal an outbreak.
2. Define and Identify Cases
To accurately track the spread of disease, epidemiologists develop a case definition—a set of standard criteria for identifying individuals affected by the disease. This case definition includes specific symptoms, diagnostic test results, or other epidemiological features, like the time period and location of exposure.
Once the case definition is established, public health officials work to identify all cases. This includes both confirmed cases (those diagnosed with laboratory evidence) and probable or suspected cases (individuals exhibiting symptoms or meeting exposure criteria).
3. Conduct Descriptive Epidemiology
Descriptive epidemiology focuses on analyzing the person, place, and time aspects of the outbreak. This step helps characterize the outbreak by answering key questions such as:
- Person: Who is affected? What are their demographic characteristics (age, sex, occupation, etc.)?
- Place: Where are the cases occurring? Are there geographic clusters or locations of concern (e.g., schools, restaurants)?
- Time: When did the outbreak begin? Is the number of cases increasing, peaking, or declining?
Using this information, epidemiologists may create epidemic curves (epi curves), which visually depict the number of cases over time, offering clues about the source and transmission of the outbreak.
4. Formulate Hypotheses
Based on descriptive data, epidemiologists develop hypotheses about the source, mode of transmission, and risk factors contributing to the outbreak. These hypotheses are guided by the outbreak’s characteristics, including who is affected and how the disease might be spreading. This stage often involves reviewing existing scientific knowledge about the disease or pathogen involved.
Example: If an outbreak of gastrointestinal illness is observed among individuals who ate at a specific restaurant, public health officials may hypothesize that a contaminated food item is the source of the outbreak.
5. Test Hypotheses through Analytical Studies
To confirm or refute these hypotheses, epidemiologists use analytical epidemiology methods. This typically involves conducting studies such as:
- Case-control studies: Comparing individuals who became ill (cases) with those who did not (controls) to identify risk factors or exposures associated with the outbreak.
- Cohort studies: Studying a group of individuals exposed to a potential source of the disease and comparing their outcomes with those who were not exposed.
The goal of these studies is to determine the likely source of the outbreak, how the disease is spreading, and what factors may be contributing to the spread. Statistical analysis is used to identify significant associations between exposures and illness.
6. Implement Control and Prevention Measures
Once the source of the outbreak is identified, public health officials implement control measures to stop the spread of disease and prevent additional cases. These interventions may include:
- Isolating or quarantining affected individuals: Keeping infected individuals away from others to reduce transmission.
- Recalling contaminated food or products: Removing harmful products from the market to prevent further exposures.
- Health education campaigns: Providing the public with information on how to protect themselves (e.g., hygiene practices, vaccination).
- Vaccination campaigns: Administering vaccines to high-risk populations if the outbreak involves a vaccine-preventable disease.
Public health agencies may also recommend closing facilities, such as schools or restaurants, if they are identified as the source of the outbreak. The success of these measures is often monitored by tracking new cases over time.
7. Communicate Findings
Throughout the outbreak investigation, public health authorities must communicate their findings to the public, healthcare providers, and policymakers. Transparency and timely communication are key to managing public perception and ensuring that control measures are followed. Reports often include:
- Press releases to inform the public about the outbreak and any preventive actions they should take.
- Scientific publications or reports that document the outbreak investigation for future reference and learning.
Example: During the COVID-19 pandemic, health authorities provided daily briefings on the number of new cases, hospitalizations, and deaths, as well as updates on government measures to control the virus’s spread.
8. Perform Ongoing Monitoring and Evaluation
Even after the outbreak appears to be under control, continued monitoring is crucial. Public health officials track the number of new cases to ensure that the outbreak is truly over and that there is no resurgence. Additionally, they evaluate the effectiveness of the interventions and, if needed, adjust strategies to prevent future outbreaks.
Types of Outbreaks Investigated
Outbreak investigations are used to respond to various types of public health threats, including:
- Infectious Disease Outbreaks: The most common type of outbreak involves infectious diseases, such as flu, measles, tuberculosis, or COVID-19. These outbreaks often spread through person-to-person contact, airborne transmission, or contaminated food and water.
- Foodborne Illness Outbreaks: Foodborne outbreaks occur when contaminated food or beverages cause illness. Common pathogens include Salmonella, E. coli, and Norovirus. Foodborne outbreaks can affect hundreds or even thousands of individuals, especially if the contamination involves widely distributed products.
- Healthcare-Associated Infections: Outbreaks can also occur in healthcare settings, where infections are transmitted within hospitals, clinics, or nursing homes. These infections may arise from poor hygiene practices, contaminated medical equipment, or the overuse of antibiotics.
- Environmental Exposures: Outbreaks may occur due to environmental hazards such as chemical spills, toxic fumes, or exposure to contaminated water. In these cases, public health officials must determine the source of exposure and implement measures to reduce harm.
Real-World Examples of Outbreak Investigations
1. The 2011 E. coli Outbreak in Germany
In 2011, Germany experienced a large outbreak of Escherichia coli (E. coli) infections, linked to contaminated fenugreek sprouts. The outbreak resulted in over 4,000 cases of illness and 50 deaths. Through epidemiological investigations, public health officials traced the outbreak to a specific batch of sprouts, leading to a product recall and public warnings to avoid consuming the contaminated food.
2. The 2014 Ebola Outbreak in West Africa
The 2014 Ebola outbreak was one of the most significant in recent history, affecting several West African countries. Epidemiologists worked tirelessly to trace the outbreak’s spread, identify transmission patterns, and implement control measures such as quarantines, travel restrictions, and mass vaccination campaigns. International collaboration and rapid response were crucial to eventually controlling the outbreak.
3. Legionnaires’ Disease Outbreak in New York City (2015)
In 2015, New York City experienced an outbreak of Legionnaires’ disease, a severe form of pneumonia caused by the Legionella bacteria. Public health officials traced the outbreak to a contaminated cooling tower in a large building, leading to the tower’s disinfection and stricter regulations for cooling system maintenance. This outbreak highlighted the importance of environmental monitoring in preventing similar incidents.
Challenges in Outbreak Investigations
While outbreak investigations are critical for public health, they can be challenging due to several factors:
- Delayed Reporting: In some cases, outbreaks are not detected until a significant number of cases have occurred, making it harder to identify the source or contain the spread.
- Data Gaps: Incomplete or inaccurate case information can hinder the ability to accurately map the spread of disease or identify risk factors.
- Multiple Sources of Exposure: When outbreaks are caused by multiple sources (e.g., different food items or modes of transmission), it can be difficult to pinpoint the root cause.
- International Coordination: In global outbreaks, coordination between countries and agencies can be complex, requiring effective communication and collaboration to manage the situation.
Conclusion
Outbreak investigations are essential for identifying, understanding, and controlling the spread of diseases. By following a structured process—verifying the outbreak, defining cases, conducting descriptive and analytical epidemiology, and implementing control measures—public health officials can minimize the impact of outbreaks and prevent future occurrences. These investigations are at the heart of public health efforts to protect populations and ensure timely, effective responses to emerging health threats.
Humanities Moment
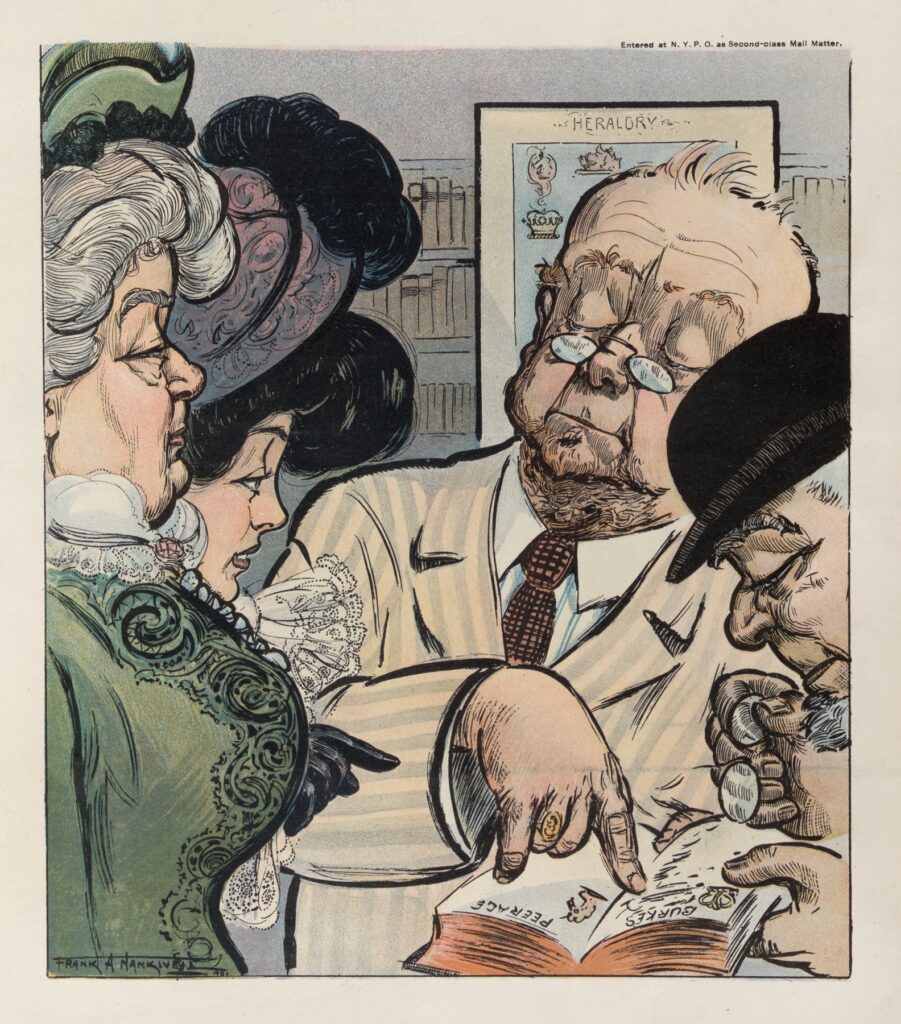
The featured image for this Epi Explained is During the investigation (1901) by Frank Arthur Nankivell (Australian, 1869–1959). Frank Arthur Nankivell was an Australian artist and political cartoonist, best known for his caricatures in Puck, America’s first successful humor magazine. Born in 1869 in Victoria, Australia, he studied art in Melbourne, worked as a cartoonist in Japan, and later moved to New York in 1896, where his influential cartoons focused on social and political subjects. Nankivell remained active in New York’s art scene until 1913 and was a member of the prestigious New York Circumnavigators Club, which included other famous personalities such as Harry Houdini and Ernest Hemingway.
Thank you for reading this installment of Epi Explained. Please check out the rest of our website for more information on Public Health Methods, Programming, and other key topics.
