Epi Explained: What are Non-Pharmaceutical Interventions (NPIs)?
Non-Pharmaceutical Interventions (NPIs) are actions, apart from medical treatments like vaccines and medications, that individuals and communities can take to help slow the spread of contagious diseases. NPIs are crucial during outbreaks and pandemics, especially when vaccines or treatments are unavailable, limited, or ineffective against the disease. These interventions include strategies such as social distancing, mask-wearing, quarantine, isolation, travel restrictions, and personal hygiene practices, all designed to reduce human-to-human transmission.
In this EpiExplained, we’ll cover the various types of NPIs, factors to consider when implementing them, the concept of social fatigue, and historical examples of NPIs in action.
Key Questions
What are Non-Pharmaceutical Interventions (NPIs)?
Non-Pharmaceutical Interventions (NPIs) are measures that individuals and communities can implement to reduce the spread of infectious diseases without the use of medical treatments such as vaccines or medications. Examples include hand hygiene, social distancing, mask-wearing, and quarantines.
Why are NPIs important during an outbreak?
NPIs are critical in controlling disease transmission, especially when vaccines or treatments are not yet available, or during the early stages of an outbreak. They help reduce the number of cases, protect healthcare systems, and limit the spread of the disease.
What factors influence the success of NPIs?
The success of NPIs depends on factors such as timing, public compliance, economic impacts, and the effectiveness of communication from health authorities. Cultural attitudes and access to resources also play a role in how well NPIs are adopted.
How can social fatigue affect NPIs?
Social fatigue occurs when individuals become tired or frustrated with prolonged restrictions, such as social distancing or mask-wearing. This can lead to reduced compliance and increased disease transmission, making it important to manage public expectations and offer support.
Can NPIs completely stop an outbreak?
NPIs can slow the spread of a disease and reduce its impact, but they are often most effective when used in combination with other public health measures, such as testing, contact tracing, and vaccination campaigns once available.
What are Non-Pharmaceutical Interventions (NPIs)?
Non-Pharmaceutical Interventions (NPIs) are measures that reduce the spread of infectious diseases without the use of pharmaceuticals, such as vaccines or antiviral medications. These interventions are often implemented to delay the spread of a disease, reduce the peak burden on healthcare systems, and protect high-risk populations. NPIs are particularly important during the early stages of an outbreak when medical countermeasures may not yet be available or widely distributed.
NPIs are not one-size-fits-all solutions. Their effectiveness depends on the type of disease, how it spreads, the population’s characteristics, and the timing and stringency of the interventions. In this article, we’ll explore the different categories of NPIs, key considerations for implementing them, their societal impact, and examples of their use throughout history.
Categories of NPIs
NPIs are generally categorized into three main types: personal protective measures, community-level measures, and environmental measures. Each category targets a different level of disease prevention, from individual actions to widespread societal changes.
1. Personal Protective Measures
Personal NPIs are actions that individuals can take to reduce their risk of contracting or spreading a disease. These are the first line of defense and are typically the most straightforward to implement, although their effectiveness can vary based on individual compliance.
Key Personal NPIs:
- Hand Hygiene: Frequent handwashing with soap and water, or using alcohol-based hand sanitizers, is one of the simplest and most effective ways to prevent disease transmission, especially for respiratory and gastrointestinal infections.
- Respiratory Etiquette: Covering coughs and sneezes with a tissue or the inside of the elbow reduces the spread of droplets that may carry viruses or bacteria.
- Face Masks: Wearing masks, particularly in crowded or enclosed spaces, can help reduce the transmission of respiratory droplets and protect both the wearer and others.
- Self-Isolation: Individuals who are symptomatic or have been exposed to a known case of the disease can self-isolate to prevent spreading it to others.
Effectiveness of Personal NPIs:
- Personal NPIs rely heavily on individual compliance and can be influenced by public perception, education, and access to resources. For example, proper mask-wearing requires both the availability of masks and correct use.
2. Community-Level Measures
Community NPIs involve larger-scale actions that affect groups of people or entire communities. These measures are usually coordinated by public health authorities or governments and aim to reduce opportunities for close contact and large gatherings, where transmission can easily occur.
Key Community-Level NPIs:
- Social Distancing: Maintaining physical space between individuals (typically 6 feet or more) reduces the likelihood of transmitting infectious diseases, particularly airborne or droplet-spread pathogens.
- Quarantine and Isolation: Quarantine separates individuals who have been exposed to a disease but are not yet symptomatic, while isolation separates those who are already sick from healthy individuals.
- School Closures: Temporarily closing schools can help reduce the spread of infections among children, who are often efficient disease transmitters. School closures also reduce transmission between households.
- Remote Work Policies: Encouraging or mandating remote work for non-essential workers reduces the number of people commuting and congregating in workplaces, which helps lower transmission rates.
- Event and Gathering Restrictions: Limiting the size of public gatherings, or canceling mass events, can prevent large-scale outbreaks, particularly in enclosed or crowded environments.
- Travel Restrictions and Border Controls: Restricting non-essential travel and implementing health checks at borders can slow the spread of diseases, especially those that may be imported from other regions. This can include closing off international borders, provincial borders, or sometimes even small scale communities. This is often seen as a last option due to its impact on the communities in question, and referred to as Cordon Sanitare (French: sanitary cordon).
3. Environmental Measures
Environmental NPIs focus on modifying physical spaces to reduce the spread of disease. These interventions often involve changes in infrastructure or environmental sanitation to limit transmission in shared environments.
Key Environmental NPIs:
- Enhanced Cleaning and Disinfection: Increasing the frequency of cleaning and disinfecting high-touch surfaces (e.g., door handles, elevator buttons) in public spaces, schools, workplaces, and transportation systems can reduce the transmission of pathogens.
- Ventilation Improvements: Improving indoor ventilation by opening windows, using air filtration systems, or modifying heating, ventilation, and air conditioning (HVAC) systems can help disperse infectious particles and lower the risk of airborne transmission.
- Physical Barriers: Installing physical barriers, such as plexiglass shields, in areas where maintaining physical distance is difficult (e.g., retail counters) can help prevent direct contact between individuals.
- Building Modifications: Creating one-way pedestrian traffic flows, widening walkways, and redesigning shared spaces can reduce close contact in places where people congregate.
Factors to Consider When Implementing NPIs
While NPIs are essential tools in controlling the spread of infectious diseases, their implementation requires careful consideration of various factors to ensure their effectiveness and minimize unintended consequences.
1. Timing and Stage of the Outbreak
The timing of NPI implementation is critical. Early intervention often yields the best results in controlling disease spread. However, if implemented too late, NPIs may not significantly affect the outbreak’s trajectory.
- Early Implementation: Introducing NPIs at the beginning of an outbreak can “flatten the curve,” slowing the disease’s spread and preventing healthcare systems from being overwhelmed.
- Delayed Implementation: Waiting too long to implement NPIs can lead to rapid disease transmission and an explosive increase in cases, making it harder to control the outbreak.
2. Compliance and Public Perception
The success of NPIs depends largely on public adherence. Factors that influence compliance include:
- Public Trust: Trust in public health authorities and government recommendations is crucial. Clear, consistent, and transparent communication fosters compliance. It should be noted that often times, the public views the actions of any government agency as “The Government”, so being cognizant of not only what your agency is doing, but of those who can be grouped in with you is essential. Often times, being able to have good relationships with community leaders can help increase public trust, but takes time and should be prioritized in a so-called Blue Sky (normal/day-to-day) environment, and not be undertaken only after something has occurred. Failure to do so can often reinforce the image of “outsiders” coming in to tell communities what to do and taking away rights, even if the intent is purely to save lives and decrease impacts of disease.
- Cultural Norms: Cultural attitudes toward certain interventions, like mask-wearing or social distancing, can affect how well NPIs are adopted. In some cultures, wearing masks in public has long been normalized, while in others, it may be viewed with skepticism or resistance.
- Access to Resources: Ensuring that individuals have the necessary resources to comply with NPIs is vital. For instance, hand hygiene requires access to clean water, soap, or hand sanitizers, and mask mandates require widespread availability of masks.
3. Economic and Social Considerations
NPIs, especially community-level and environmental interventions, often have economic and social implications that need to be weighed against their public health benefits.
- Economic Impact: Measures like business closures, travel bans, and remote work mandates can have significant economic consequences, particularly for industries reliant on physical interaction, such as hospitality, tourism, and retail. However, this should always be considered alongside the very real cost in human lives of prioritizing business interests over appropriate NPI implementation.
- Equity Issues: Some NPIs may disproportionately affect certain populations, particularly low-income communities, essential workers, and those without access to healthcare or paid sick leave. Governments must ensure that vulnerable groups are supported during NPI implementation, such as providing financial aid, social services, adequate protective equipment, etc.
- Educational Disruptions: School closures, while effective in controlling outbreaks, can disrupt learning, particularly for students in disadvantaged communities who may lack access to online education or resources.
Social Fatigue and NPI Sustainability
What is Social Fatigue?
One of the key challenges of long-term NPI implementation is social fatigue. As NPIs, such as social distancing, mask-wearing, and travel restrictions, remain in place for extended periods, individuals and communities may experience psychological and emotional fatigue. This can lead to reduced compliance, even if the measures are still necessary to control disease transmission.
Factors Contributing to Social Fatigue:
- Duration of Restrictions: The longer NPIs are in place, the more likely people are to feel frustrated, anxious, and isolated, leading to non-compliance. People may begin to disregard recommendations, such as avoiding large gatherings, as they become fatigued by the restrictions.
- Lack of Clear Communication: When public health messaging is inconsistent or unclear, it can lead to confusion and reduce public trust in the measures. People may question the effectiveness or necessity of NPIs, especially if they do not see immediate results. Clear Communication should also not be confused with keeping to only one message, especially if the information is out of date or ineffective. Acknowledging a changing landscape and taking ownership of decisions, and communicating that as well, can increase public trust and adherence.
- Social and Economic Pressures: Prolonged NPIs can strain social networks, economic livelihoods, and mental health. Job losses, financial stress, and isolation from loved ones contribute to social fatigue and increase the desire to return to normal activities.
- Perceived Ineffectiveness: If the disease persists despite NPIs, some individuals may view the interventions as ineffective and stop following them, even if those measures are still critical to controlling the outbreak.
Strategies to Mitigate Social Fatigue:
- Targeted Messaging: Clear, consistent, and evidence-based communication about the importance of NPIs is essential. Public health authorities should explain the rationale behind interventions, update the public regularly, and provide a timeline or benchmarks for lifting restrictions.
- Balancing Restrictions with Flexibility: Authorities should seek a balance between necessary restrictions and social flexibility. For example, allowing outdoor activities with safety measures in place can provide individuals with a sense of normalcy without compromising public health.
- Mental Health Support: Offering mental health services, promoting community engagement (virtually or safely in-person), and encouraging physical activity can help alleviate some of the emotional and psychological burdens of prolonged NPIs.
Historical Examples of NPIs
Throughout history, NPIs have been used to combat infectious diseases long before modern medicine developed effective vaccines or treatments. Here are some notable examples of NPIs in action:
1. The 1918 Influenza Pandemic
During the 1918 influenza pandemic, also known as the Spanish flu (despite having an origination point in Kansas, United States), NPIs such as social distancing, quarantines, and the use of masks were implemented in many cities worldwide to slow the spread of the virus. The pandemic, which killed an estimated 50 million people globally, showcased both the strengths and limitations of NPIs.
- Success Stories: Cities like St. Louis implemented strict social distancing measures early in the outbreak and were able to reduce peak mortality rates significantly. Public health campaigns promoted mask-wearing, and schools, theaters, and businesses were temporarily closed.
- Challenges: Other cities, such as Philadelphia, delayed the implementation of NPIs, leading to devastating surges in cases and overwhelming healthcare systems.
2. The SARS Outbreak of 2003
The SARS (Severe Acute Respiratory Syndrome) outbreak in 2003 demonstrated the importance of NPIs in containing a highly contagious and deadly respiratory virus. SARS spread to 26 countries, but through aggressive implementation of NPIs, including isolation, quarantine, travel restrictions, and contact tracing, the outbreak was largely contained within a few months.
- Quarantine and Isolation: Quarantining suspected cases and isolating confirmed patients were central to controlling SARS. The rapid identification and isolation of cases prevented widespread community transmission.
- Global Coordination: Countries worked together to implement NPIs at a global level, particularly in restricting travel and screening individuals at borders, which limited the spread of the virus across borders.
3. The COVID-19 Pandemic (2020-Present)
The COVID-19 pandemic is perhaps the most well-known example of NPIs being deployed on a global scale. With no available vaccine or specific treatment in the early months of the pandemic, NPIs became the primary strategy for controlling the spread of the SARS-CoV-2 virus.
- Widespread Lockdowns: Countries around the world implemented varying levels of lockdowns, including school and business closures, stay-at-home orders, and bans on public gatherings. These measures helped reduce transmission, but also had significant social and economic impacts.
- Mask Mandates: The widespread use of masks, particularly in indoor and crowded settings, was promoted as an essential NPI to reduce airborne transmission of the virus. Public health messaging and government mandates varied widely between regions, leading to differences in compliance.
- Travel Bans and Quarantines: Many countries implemented strict travel restrictions, including mandatory quarantine for incoming travelers and bans on non-essential international travel, which helped limit cross-border transmission.
Conclusion
Non-Pharmaceutical Interventions (NPIs) are critical tools in the control of infectious disease outbreaks, especially when vaccines or treatments are unavailable or insufficient. From personal actions like hand hygiene and mask-wearing to community-wide measures like social distancing, quarantine, and travel restrictions, NPIs have been proven effective in reducing transmission.
However, implementing NPIs requires careful consideration of timing, compliance, social impacts, and other consequences. Long-term reliance on NPIs can also lead to social fatigue, making it essential for public health officials to balance restrictions with maintaining public trust and keeping the public adequately engaged and informed.
Historically, NPIs have been used successfully to combat pandemics like the 1918 influenza, SARS in 2003, and COVID-19. Their continued relevance highlights the importance of preparedness and public health infrastructure in addressing future outbreaks.
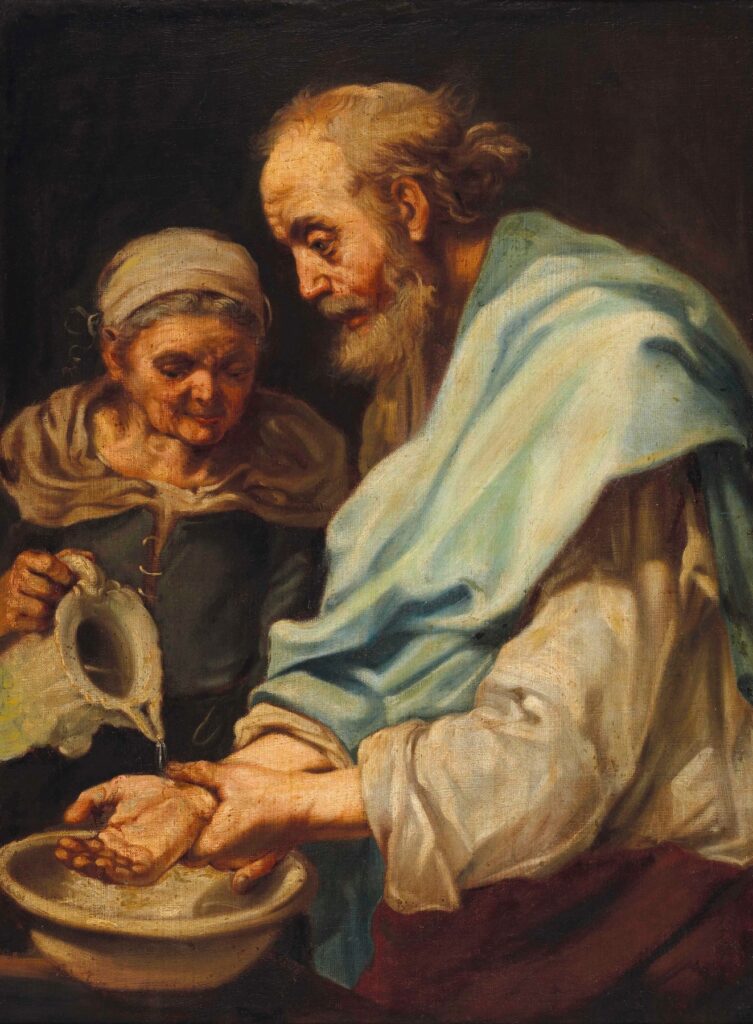
Humanities Moment
The featured image for this Epi Explained is The Hand Washing (Allegory of Water) by Bernhard Keil (Danish, 1624-1687). Bernhard Keil, also known as Keyl, was a Danish Baroque painter born in Helsingør who became a pupil of Rembrandt. After studying with Danish painter Morten Steenwinkel and later working in Amsterdam, Keil established his own workshop before traveling to Rome in 1656, where he worked until his death in 1687. His work was influenced by Jan Lievens, and he, in turn, influenced artists such as Pietro Bellotti, Antonio Cifrondi, and Giacomo Francesco Cipper. Keil also worked in Bergamo and Venice during his career.
Thank you for reading this very extended Epi Explained article. If you’d like to check out our other topics, a browse through our website would be greatly appreciated!
