Gut Health and Endometriosis: New Study Uncovers Biomarkers for Non-Invasive Diagnosis
Key Takeaways
- A new study reveals distinct stool metabolites in women with endometriosis, offering a pathway for non-invasive diagnosis.
- The study identifies 4-hydroxyindole as a promising therapeutic candidate that reduces endometriosis-related inflammation and pain.
- The findings suggest a connection between endometriosis and inflammatory bowel disease (IBD), revealing shared gut microbiota patterns.
- This research emphasizes the importance of gut health in the diagnosis and management of endometriosis.
Introduction
Endometriosis is a chronic gynecological condition that affects approximately 10% of women of reproductive age globally, causing pelvic pain, inflammation, and infertility. Despite its prevalence, diagnosing endometriosis is challenging, often requiring invasive procedures like laparoscopy. New research, published in Med, offers hope by identifying gut microbiota-derived biomarkers that could revolutionize diagnosis and treatment.
The study, led by researchers at Baylor College of Medicine, explored the microbiota-metabolite signatures in stool samples from women with and without endometriosis. Their findings provide evidence for non-invasive diagnostic methods and highlight the therapeutic potential of gut-derived compounds, such as 4-hydroxyindole, in reducing disease progression and pain.
The Study and Methodology
The study involved stool sample analysis from 18 women with endometriosis and 31 control participants. Researchers used high-throughput metabolomics and bacterial sequencing techniques to identify differences in gut-derived metabolites. The analysis revealed 61 metabolites that differed significantly between the two groups, with 4-hydroxyindole (4HI) emerging as a key compound.
Functional studies were conducted using patient-derived cells and murine models of endometriosis. These experiments demonstrated that 4HI inhibits the growth of endometriotic lesions and alleviates pain in animal models, supporting its potential as a therapeutic intervention for managing endometriosis.
Microbiota-Driven Metabolites and Their Role in Endometriosis
The gut microbiome plays a crucial role in regulating inflammation and immune function, both of which are central to the progression of endometriosis. The study found that women with endometriosis exhibited reduced levels of beneficial bacteria, such as Faecalibacterium and Lachnospiraceae. In contrast, pro-inflammatory bacterial populations, including Streptococcus and Actinomyces, were elevated.
The presence of these altered microbial profiles correlated with changes in metabolite production, particularly the reduction of 4HI. This compound, primarily derived from gut bacteria, was shown to inhibit lesion formation and reduce inflammation, suggesting a protective role in endometriosis management.
Link Between Endometriosis and Inflammatory Bowel Disease (IBD)
One of the most intriguing findings of the study is the overlap between the gut microbiota profiles of women with endometriosis and those with IBD. Both conditions share common symptoms, including chronic inflammation, altered gut microbiota, and heightened immune responses.
This connection suggests that endometriosis and IBD may have overlapping mechanisms related to gut health. Understanding this link could lead to more targeted interventions and improve the diagnosis of endometriosis, which is often misdiagnosed as IBD due to similar symptoms.
Implications for Non-Invasive Diagnosis
The identification of distinct stool metabolites opens the door to non-invasive diagnostic tools for endometriosis. Current diagnostic methods are invasive, time-consuming, and often lead to delayed treatment. The use of stool-based biomarkers, such as those identified in this study, could revolutionize diagnosis by providing a quick, accessible, and reliable way to detect the disease.
In addition to improving diagnostic accuracy, non-invasive testing could reduce the emotional and physical burden on patients, leading to earlier intervention and better health outcomes.
Potential for Microbiota-Based Therapies
The discovery of 4-hydroxyindole as a therapeutic candidate is a significant step toward developing microbiota-based treatments for endometriosis. In animal models, 4HI reduced lesion size, decreased macrophage infiltration, and alleviated pain. These findings highlight the potential for using gut-derived metabolites to modulate immune responses and manage symptoms.
Future therapies could focus on restoring healthy gut microbiota through diet, probiotics, or targeted supplements. This approach would not only address the symptoms of endometriosis but also improve overall gut health, potentially reducing the risk of other inflammatory conditions, such as IBD.
Potential Implications for Public Health Practice
The development of a non-invasive, stool-based diagnostic method for endometriosis could transform public health efforts by encouraging more individuals to seek testing. Since endometriosis often goes undiagnosed due to invasive procedures and the normalization of symptoms like pelvic pain, a simpler diagnostic tool could lower barriers to care and improve health equity for those individuals assigned female at birth. Early and accessible testing could lead to improved detection rates, providing a clearer picture of the true incidence and prevalence of endometriosis. With more comprehensive data, public health systems can better allocate resources, raise awareness, and promote early interventions, ultimately improving outcomes for individuals affected by this chronic condition. This proactive approach may also highlight the connection between gut health and gynecological disorders, emphasizing the importance of holistic health monitoring.
Conclusion
The findings from this study represent a significant advancement in the understanding of endometriosis and its relationship with gut health. By identifying distinct stool metabolites and demonstrating the therapeutic potential of 4-hydroxyindole, the research offers new avenues for non-invasive diagnosis and innovative treatments.
For public health professionals and clinicians, these insights highlight the importance of considering gut health in the management of endometriosis. Implementing stool-based diagnostics and promoting microbiota-targeted therapies could improve outcomes for millions of assigned female at birth individuals affected by this debilitating condition. Likewise, this could lower the barrier for appropriate diagnosis of a condition too often ignored.
Further research is needed to validate these findings in larger cohorts and explore the long-term effects of microbiota-based interventions. However, the potential impact on diagnosis, treatment, and quality of life makes this an exciting development in the field of women’s health.
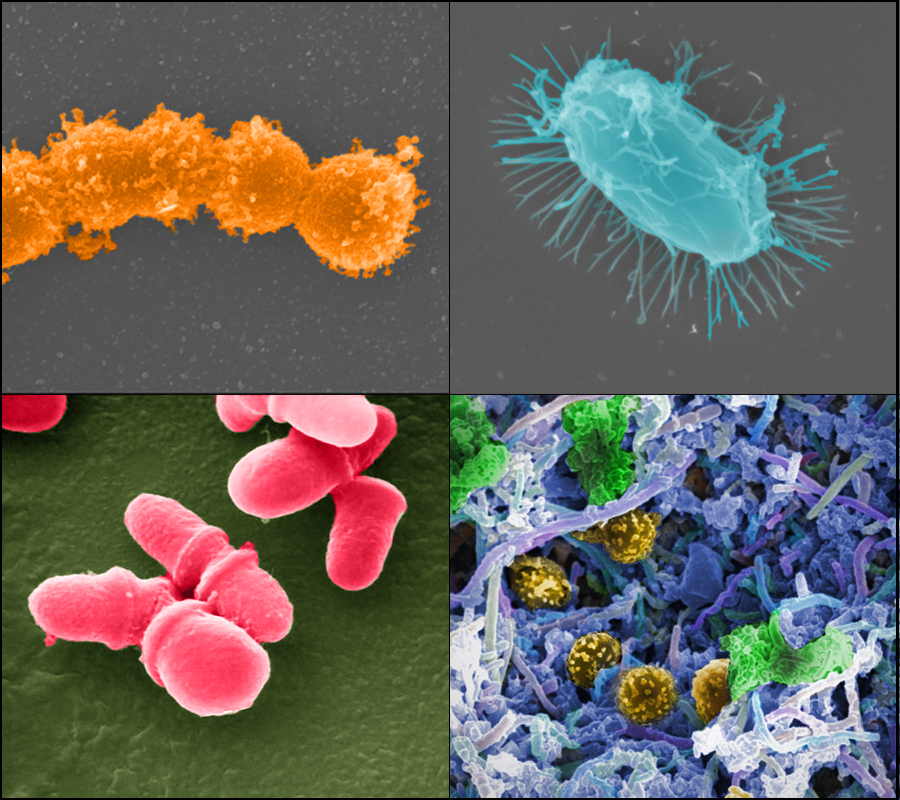
The featured image for this article is from the NIH’s Human Microbiome Project’s Flickr page.
