Evidence-Based Approaches to Public Health: Epidemiology – Causality: Causal Inference in Public Health Research
In this tutorial, we will explore the concept of causal inference in public health research. Causal inference refers to the process of determining whether an observed association between an exposure and an outcome reflects a true causal relationship. This process is essential in epidemiology because public health interventions rely on accurate identification of causal factors that impact health outcomes. Understanding causal inference is key for the Certified in Public Health (CPH) exam and for interpreting research that informs public health decisions.
By the end of this tutorial, you will understand the importance of causal inference, the methods used to establish causality, and the challenges involved in determining causality in public health research. Practice questions are included to reinforce your knowledge.
Table of Contents:
- Introduction to Causal Inference
- Why is Causal Inference Important in Public Health?
- Challenges in Establishing Causality
- Methods for Causal Inference
- Experimental Studies (Randomized Controlled Trials)
- Observational Studies (Cohort and Case-Control Studies)
- Statistical Methods for Adjusting for Confounding
- Hill’s Criteria for Causation
- Practice Questions
- Conclusion
1. Introduction to Causal Inference
Causal inference refers to the process of determining whether an exposure causes an outcome. It involves evaluating whether changes in one variable (e.g., smoking) lead to changes in another variable (e.g., lung cancer). While observational studies often reveal associations between exposures and outcomes, they do not necessarily imply causality. Causal inference requires careful consideration of the evidence and the use of appropriate methods to rule out alternative explanations such as confounding, bias, or random chance.
2. Why is Causal Inference Important in Public Health?
In public health, understanding the cause of health outcomes is critical for designing effective interventions and policies. If we can identify a true cause of a health issue, we can take action to prevent it. However, if the cause is incorrectly identified due to improper causal inference, interventions may be ineffective or even harmful. For example, knowing that smoking causes lung cancer has led to significant public health campaigns and policies to reduce smoking rates, saving countless lives.
Accurate causal inference allows public health professionals to:
- Implement effective interventions to reduce disease and improve health.
- Allocate resources efficiently to address the true causes of health problems.
- Avoid the implementation of ineffective or harmful interventions based on incorrect assumptions.
3. Challenges in Establishing Causality
Establishing causality in public health research can be difficult due to several challenges:
- Confounding: A confounder is a variable that is associated with both the exposure and the outcome, which can distort the observed relationship. For example, age might confound the relationship between physical activity and heart disease if older individuals are less active and more prone to heart disease.
- Bias: Bias can distort study results in various ways, including selection bias (when the sample is not representative) and information bias (when data are collected or measured inaccurately).
- Reverse Causality: Sometimes, the outcome may influence the exposure, rather than the exposure influencing the outcome. For example, individuals with undiagnosed heart disease may reduce their physical activity due to fatigue, creating a false association between low physical activity and heart disease.
- Ethical Constraints: In many cases, it is unethical to conduct experiments that would provide the most definitive evidence for causality. For instance, exposing people to harmful substances in a randomized controlled trial (RCT) would be unethical.
4. Methods for Causal Inference
Several methods are used to establish causal relationships in public health research. While no single method can definitively prove causality, the combination of evidence from multiple sources strengthens the case for a causal relationship.
4.1 Experimental Studies (Randomized Controlled Trials)
Randomized controlled trials (RCTs) are considered the gold standard for establishing causality. In RCTs, participants are randomly assigned to receive either an intervention or a control (e.g., placebo). Randomization helps to evenly distribute confounders across the groups, reducing the risk of bias and allowing researchers to draw stronger conclusions about the causal effect of the intervention on the outcome.
However, RCTs are often impractical or unethical in public health research, especially for harmful exposures like smoking or pollution.
4.2 Observational Studies (Cohort and Case-Control Studies)
Cohort studies and case-control studies are the most common types of observational studies used in public health research. While these studies cannot definitively establish causality, they provide valuable evidence about associations between exposures and outcomes.
- Cohort Studies: Follow a group of individuals over time to assess whether exposure to a risk factor increases the likelihood of developing an outcome. They are useful for establishing temporality (i.e., the exposure precedes the outcome).
- Case-Control Studies: Compare individuals with a disease (cases) to those without the disease (controls) to assess whether past exposure to a risk factor is associated with the disease. These studies are useful for studying rare diseases but are prone to recall bias.
4.3 Statistical Methods for Adjusting for Confounding
Confounding can distort the relationship between an exposure and an outcome, making it appear that there is a causal relationship when there is not. To address confounding, researchers use statistical methods to adjust for confounders and isolate the effect of the exposure.
- Multivariable regression: Involves including potential confounders as covariates in the model to control for their effects.
- Stratification: Analyzing the data within strata (e.g., age groups) to control for confounding and better understand the exposure-outcome relationship.
- Propensity score matching: A method that matches individuals with similar characteristics to create groups that are comparable with respect to confounders.
4.4 Hill’s Criteria for Causation
Hill’s criteria for causation provide a framework for evaluating whether an observed association is likely to be causal. These nine criteria include:
- Strength of association: A strong association is more likely to be causal than a weak one.
- Temporality: The exposure must occur before the outcome for a causal relationship to exist.
- Consistency: Repeated observations of the association in different studies and populations strengthen the case for causality.
- Biological gradient: A dose-response relationship, where greater exposure leads to greater risk, supports causality.
- Plausibility: The association should make biological sense based on current scientific knowledge.
- Coherence: The association should align with what is already known about the disease.
- Specificity: The exposure leads to a specific outcome, although this is not always necessary.
- Experiment: Experimental evidence, such as from RCTs, can provide strong support for causality.
- Analogy: If a similar exposure is known to cause the outcome, it supports the likelihood of a causal relationship.
5. Practice Questions
Test your understanding of causal inference with these practice questions. Try answering them before checking the solutions.
Question 1:
A study finds that individuals who exercise regularly have a lower risk of heart disease. However, individuals who exercise may also eat healthier diets and be wealthier. What issue does this example highlight?
Answer 1:
Answer, click to reveal
This example highlights the issue of confounding, where factors such as diet and wealth may influence the relationship between exercise and heart disease, potentially distorting the observed association.
Question 2:
A randomized controlled trial finds that a new medication reduces blood pressure in individuals compared to a placebo. What method was used to minimize confounding in this study?
Answer 2:
Answer, click to reveal
Randomization was used to minimize confounding by evenly distributing potential confounders across the treatment and placebo groups.
Question 3:
A researcher uses multivariable regression to adjust for age and smoking status when examining the relationship between alcohol consumption and liver disease. What is the researcher trying to control for?
Answer 3:
Answer, click to reveal
The researcher is trying to control for confounding by adjusting for age and smoking status, which could influence the relationship between alcohol consumption and liver disease.
6. Conclusion
Causal inference is a critical process in public health research, allowing researchers to determine whether observed associations are truly causal. While it is challenging to establish causality, the combination of evidence from randomized controlled trials, observational studies, and statistical methods can provide strong support for causal relationships.
Remember:
- Randomized controlled trials provide the strongest evidence for causality by minimizing confounding and bias.
- Observational studies are useful for identifying associations, but they require careful consideration of confounding and bias.
- Statistical methods such as multivariable regression and stratification help control for confounding and provide more accurate estimates of causal effects.
- Hill’s criteria for causation offer a framework for evaluating whether an observed association is likely to be causal.
Final Tip for the CPH Exam:
Make sure you understand the various methods used for causal inference and the challenges involved in establishing causality. Practice applying these methods to different research scenarios, as this knowledge is crucial for answering questions related to causality in the Certified in Public Health (CPH) exam.
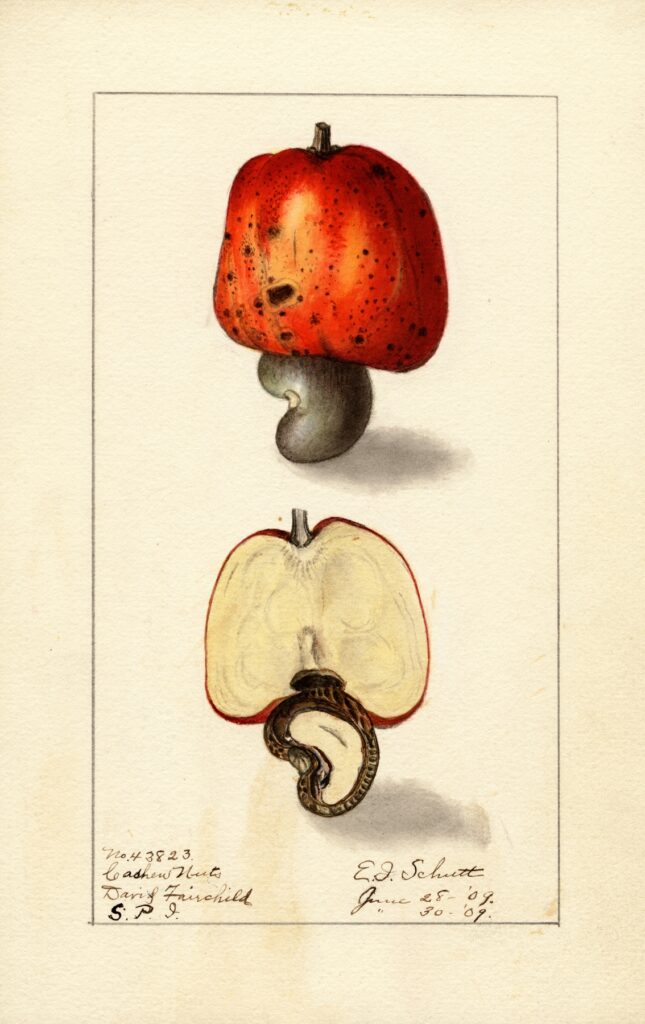
Humanities Moment
The featured image for this CPH Focus is Anacardium occidentale (1909) by Ellen Isham Schutt (American, 1873 – 1955). Schutt was an American botanical illustrator renowned for her contributions to the U.S. Department of Agriculture’s Pomological Watercolor Collection, painting over 700 detailed watercolors of fruits and nuts. Born in Arlington, Virginia, she was also an early resident of Cherrydale, where she built a notable neoclassical home and contributed to genealogical research. Her precise illustrations, often highlighting fruit imperfections, supported agricultural studies and reflected Progressive Era ideals of nature control. Later, she painted an extensive series of apples for the University of California and modeled fruit in wax to study preservation. Schutt’s legacy endures through her detailed botanical art.
