This article was written in collaboration and using interview material from Morgie Bee. All edits, additions or modifications were minimal in nature and approved by Morgie prior to publishing, to ensure their voice was front and center. Alongside here, you can find Morgie on BlueSky at @morgiebeeva.bsky.social , sewing absolute chaos on their Twitch Channel as the appropriately named Plague Babi, or playing various roles in Audio Dramas produced by Twin Strangers Productions.
Community Experts Issue 1: Navigating POTS and Long COVID – Morgie’s Story
The Early Signs of POTS
Morgie’s story begins during the height of the COVID-19 pandemic, when they contracted the virus multiple times despite being vaccinated.
After their second and most severe bout in early 2021, Morgie began experiencing persistent and unexplained symptoms:
“After a couple weeks of recovery though I was back at work but never felt the same. This was around January of 2021, at the time I was trying out new medications for
my mental health so I wrote off my symptoms as side effects.”
As the months passed, these symptoms became harder to ignore. A near-fainting episode at work in June 2021 landed Morgie in the hospital, where blood tests revealed dangerously low blood sugar and electrolytes. Despite being stabilized, they were sent home without a diagnosis. It wasn’t until a nurse mentioned Long COVID that Morgie began connecting the dots:
“It took the nurse looking at me and going, ‘honey, someone who is 21 shouldn’t feel like this, I really think you should look into long COVID symptoms,’ for it to click that something was definitely wrong with me.”
Drawing on their medical background and personal determination, Morgie began researching their symptoms. Eventually, they found information about POTS, a condition that affects blood flow and causes symptoms like rapid heart rate, dizziness, and fainting when standing.
Pushing for a Diagnosis
Getting a diagnosis for POTS often requires persistence, as Morgie’s story illustrates. Recognizing the signs in their own body, they advocated for themselves during a cardiology appointment:
“We had me wear a heart monitor and there were several times where tachycardia was seen. I recall once my heart rate even went up to 210 and I got a call. I was just
standing at work and felt pretty uneasy. When we had our follow-up appointment I brought up POTS to [the cardiologist], and we concluded that I met the diagnostic
criteria by doing the ‘poor man’s’ tilt table test.”
While Morgie finally had a name for their condition, the relief of diagnosis was short-lived:
“She told me that she believed I was correct but that she had no idea how to treat me and advised me to go to the one specialist who knew. His waitlist was years long though, and not covered by my insurance. So now I knew what I had but was basically left out to dry.”
Living with POTS
Managing POTS requires significant lifestyle changes, and for Morgie, these adaptations have been both necessary and challenging:
“I managed my symptoms the best I could, got a note to sit at work periodically and for the most part everything was okay. I had a few bad days a month but could stand for about four hours.”
However, their condition worsened after another COVID-19 infection in early 2023. By August of that year, Morgie’s baseline had shifted dramatically:
“I woke up one day barely able to stand for more than 5 minutes, my heart rate is in the 180s. It was clear my baseline had shifted dramatically. I went on a leave of absence from work, later having to quit my job.”
Now, Morgie navigates life with severe limitations, including being unable to stand for more than 30–45 minutes on a good day. Despite their efforts to seek care, systemic barriers and stigma have left them feeling abandoned by the healthcare system.
Barriers to Care for POTS Patients
Morgie’s experience reflects the broader challenges faced by many POTS patients. They describe dismissive attitudes from healthcare providers, especially in the context of their mental health history:
“It’s pretty common knowledge that a lot of POTS patients will get misdiagnosed with anxiety… Even with my POTS diagnosis, a lot of my symptoms will get dismissed,
or doctors will try to treat my anxiety even though I’m saying these symptoms are from my POTS.”
This dismissal is compounded by other systemic factors, including weight stigma and insurance limitations:
“I know for a fact that if I was an acceptable BMI, my quality of care would increase… Since no longer working, I was without insurance then switched to Medicaid,
which doesn’t exactly have the best selection of specialists to get help from.”
These barriers leave many patients, including Morgie, feeling hopeless:
“Why would anyone do something like this for attention? It’s exhausting and makes me want to even stop trying to get treatment.”
POTS and the Overlap with Mental Health
For Morgie, one of the most frustrating aspects of living with POTS is the way their mental health diagnoses shape how they are treated by doctors:
“Because anxiety is on my records, the speed I get dismissed is astonishing. It feels like anxiety is the easier condition to treat—just throw a few meds at me and surely it will all be fine, right? Even though I know my body more than any doctor can, and I know for a fact it’s my POTS.”
Morgie emphasizes the need for providers to listen to patients and differentiate between mental and physical symptoms:
“Having something for 12 years, you become extremely familiar with how it affects you… Ignoring the problem doesn’t make it go away.”
A Call to Action for Healthcare Providers
Morgie’s message to healthcare providers is clear: patients need to be heard and respected, especially when dealing with complex conditions like POTS:
“I invite you to not get so upset when a patient has gone to ‘doctor Google’ and maybe explore what they are saying. Even if they are wrong… at the very least they feel heard. It is the feeling of not being heard that becomes so frustrating and feels so hopeless.”
They stress the importance of recognizing patients’ expertise in their own bodies:
“Patients 9/10 will know their body more than you will. Sure, they may not understand the terminology, but they feel it.”
Morgie’s reflections challenge us to create a healthcare system that values collaboration, empathy, and trust.
The Urgency of Change
Morgie’s experience with POTS sheds light on the systemic failures that make it difficult for patients to receive adequate care. Their story underscores the need for:
- Increased awareness and education about POTS among healthcare providers. A link to JHU’s article for POTS is here.
- Accessible care for chronic illness patients, regardless of insurance or socioeconomic status.
- Empathy and respect for patients, particularly those with intersecting stigmas, such as mental health diagnoses or weight-related concerns.
As Morgie notes:
“The lengths, time, and money it takes to actually get help are something that really needs to be changed.”
Their journey reminds us of the urgent need to bridge gaps in care for patients with POTS and other chronic illnesses. Community Experts is committed to amplifying stories like Morgie’s to inspire meaningful change in the healthcare system.
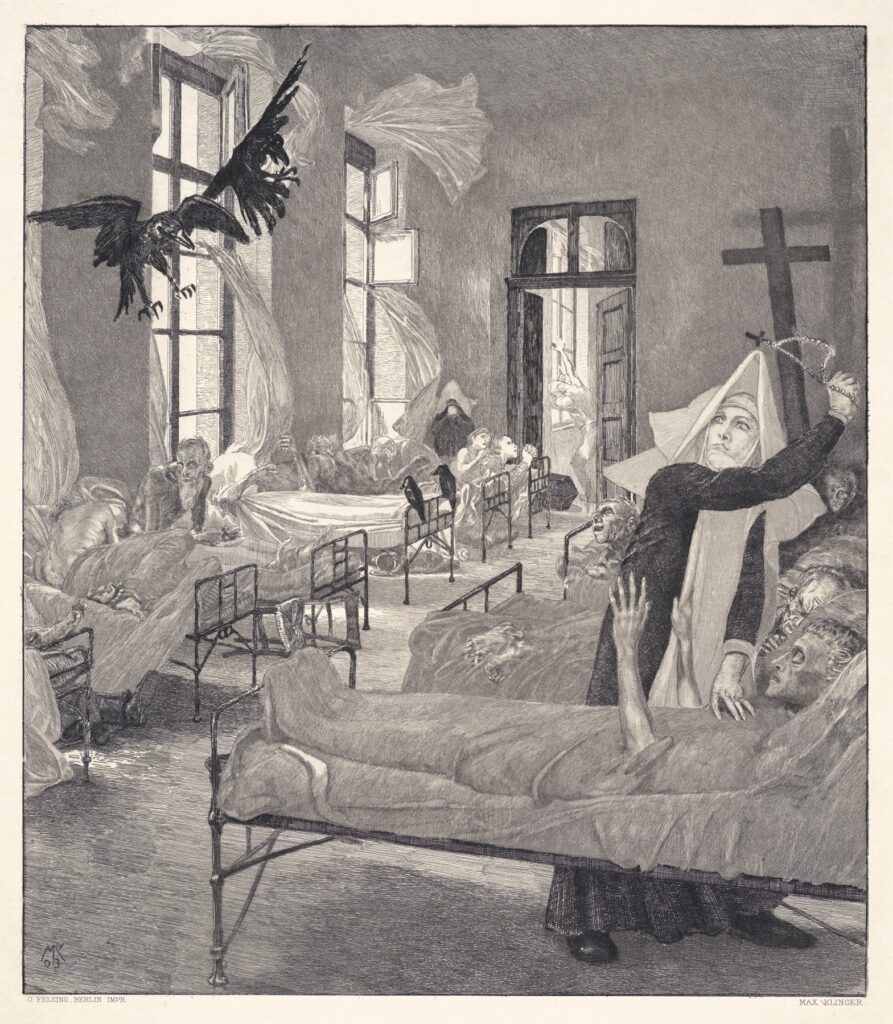
The featured image for this Community Experts interview is Plague (Pest) (1898) by Max Klinger (German, 1857-1920).
