Managing Buprenorphine-Induced Withdrawal: Challenges in Treating Patients Using Fentanyl – A Public Health Perspective
Key Takeaways
- Approximately 11.5% of patients treated with buprenorphine for opioid use disorder (OUD) developed precipitated withdrawal, with a higher rate in patients using fentanyl.
- High body mass index (BMI) and elevated urine fentanyl concentration were significantly associated with a higher risk of precipitated withdrawal.
- Precipitated withdrawal (PW) during buprenorphine initiation poses a barrier to successful treatment and retention in care for individuals using fentanyl.
- New treatment approaches, such as tailored dosing strategies, are needed to reduce PW risk and improve treatment outcomes for vulnerable populations.
Introduction
Buprenorphine is a cornerstone in the treatment of opioid use disorder (OUD), providing a safe and effective pathway for individuals to reduce opioid dependence. However, when administered to patients recently using potent opioids like fentanyl, buprenorphine can induce precipitated withdrawal (PW), a rapid and severe withdrawal syndrome that significantly impacts patient outcomes. A recent study published in JAMA Network Open has shed light on the incidence of PW among hospitalized patients using fentanyl and identified key factors associated with increased risk.
Study Overview: Risk Factors and Incidence of Precipitated Withdrawal
The study, conducted across three academic hospitals in Philadelphia from January 2020 to December 2021, focused on individuals with OUD treated with buprenorphine while admitted to emergency or hospital settings. Of the 226 patients included, 11.5% experienced PW after buprenorphine initiation. Among patients confirmed to be using fentanyl, the rate of PW increased to 16.3%, highlighting a critical challenge in treating OUD in the context of today’s increasingly fentanyl-adulterated opioid supply.
Defining Precipitated Withdrawal
PW occurs when buprenorphine, a partial agonist at the opioid receptor, displaces full agonists like fentanyl from the receptors. This sudden shift can trigger an abrupt withdrawal response, especially if fentanyl is still actively influencing the receptors due to prolonged bioaccumulation. PW was defined in this study as an increase of 5 or more points on the Clinical Opiate Withdrawal Scale (COWS) within 4 hours of buprenorphine administration.
Factors Associated with Increased Risk of PW
1. Body Mass Index (BMI)
Patients with a BMI of 30 or greater had a significantly higher risk of experiencing PW compared to those with lower BMI values. This association is likely related to the retention of fentanyl in adipose tissues, which slows its clearance from the body, thereby increasing the risk of PW even after patients show signs of withdrawal readiness.
2. Urine Fentanyl Concentration
Patients with a high concentration of fentanyl in their urine (≥200 ng/mL) were also more likely to develop PW. This suggests that the presence of residual fentanyl in the body continues to exert opioid-like effects even when withdrawal symptoms are present, complicating the initiation of buprenorphine treatment.
Challenges in Treating Opioid Use Disorder in the Fentanyl Era
The rise of fentanyl as the dominant opioid in the unregulated drug supply has complicated efforts to initiate buprenorphine treatment safely. Patients using fentanyl often face a prolonged period of withdrawal readiness due to fentanyl’s ability to persist in adipose tissue and slow clearance rates. This phenomenon has led to an increase in PW incidents, creating significant barriers for individuals attempting to engage with OUD treatment.
Fear of experiencing PW is a well-documented reason why many individuals avoid starting buprenorphine, despite its benefits in reducing opioid use and overdose mortality. PW not only creates immediate distress but also decreases trust in the treatment process and often leads to premature discontinuation of care.
Recommendations for Improving Treatment Safety and Efficacy
1. Tailored Dosing Strategies for Buprenorphine
Given the high risk of PW among individuals with elevated BMI and fentanyl exposure, healthcare providers are encouraged to consider tailored dosing strategies when initiating buprenorphine. This may involve starting with lower buprenorphine doses and titrating gradually, or using adjunct medications to mitigate withdrawal symptoms.
2. Utilizing Point-of-Care Testing for Fentanyl Levels
Point-of-care urine fentanyl tests could help providers better assess a patient’s risk for PW before starting buprenorphine. By identifying those with high residual fentanyl concentrations, clinicians can make more informed decisions about dosing and timing to minimize withdrawal risks.
3. Enhancing Provider Training and Patient Education
Training healthcare providers in the complexities of treating OUD in the fentanyl era is crucial. Clinicians should be aware of the potential for PW, particularly in patients with high fentanyl levels or higher BMIs, and should be prepared to adjust treatment plans accordingly. Additionally, educating patients about the risks and benefits of buprenorphine, along with realistic expectations, can foster better treatment adherence.
Implications for Public Health and Policy
PW is more than a medical issue; it is a public health challenge that affects retention in OUD care and the overall success of opioid addiction treatment programs. Addressing the factors associated with increased PW risk—such as high BMI and residual fentanyl levels—requires both clinical innovation and systemic changes in how addiction treatment is approached. Expanding access to medication-assisted treatment (MAT), improving training for healthcare providers, and supporting harm reduction initiatives are all critical components of a comprehensive response.
Conclusion
The findings of this study highlight the complexity of treating opioid use disorder in an era dominated by fentanyl. With nearly 12% of patients developing PW during buprenorphine initiation and even higher rates among those using fentanyl, it is clear that tailored approaches are needed to ensure safe and effective treatment. Addressing the risks associated with buprenorphine initiation requires a combination of personalized care, enhanced provider training, and systemic support to reduce the barriers individuals face in accessing lifesaving treatments.
Buprenorphine remains a critical tool in combatting the opioid crisis, but its use must be adapted to the current challenges posed by fentanyl. By understanding and mitigating the risks of precipitated withdrawal, healthcare providers can improve outcomes for patients, reduce the stigma of treatment, and contribute to the broader fight against the opioid epidemic.
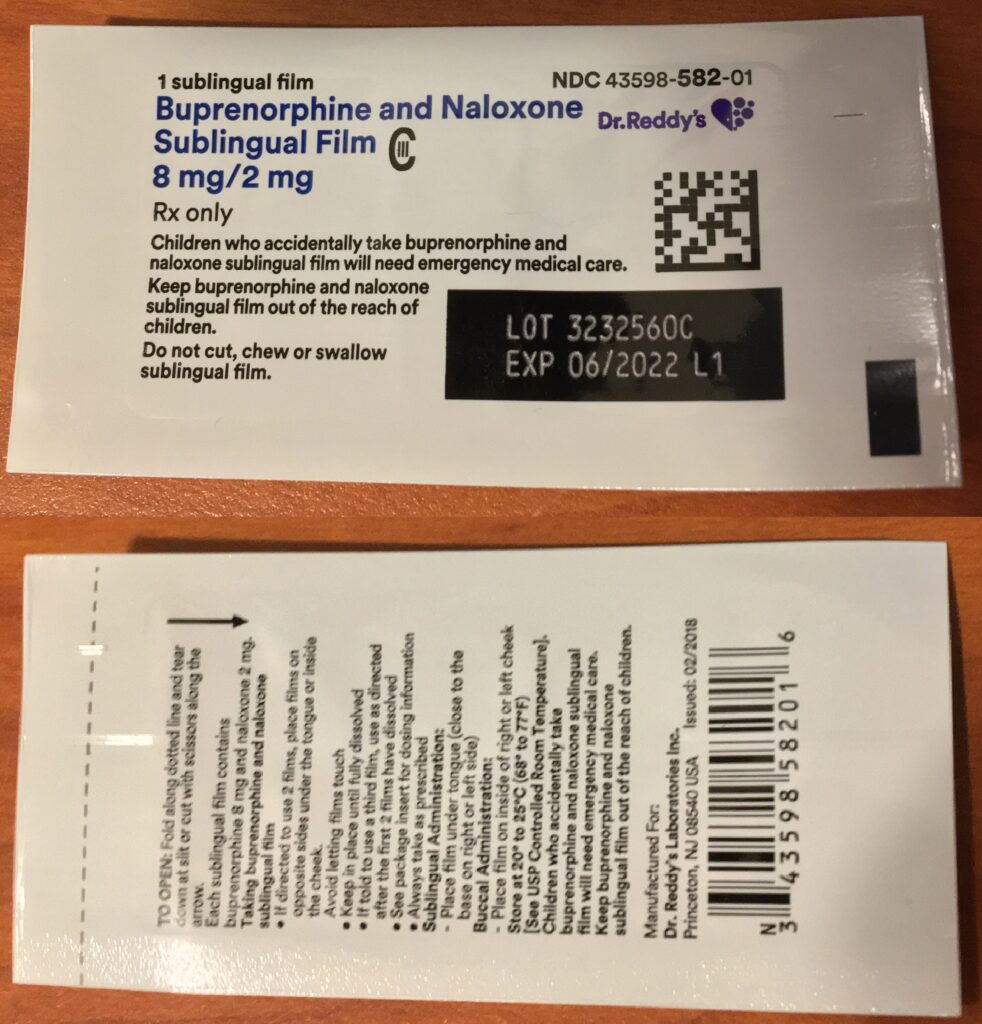
The featured image for this article is sourced from Wikimedia Commons.
